Chronic pelvic pain in Men
Chronic pelvic pain has been the subject of previous pain snippets information sheets. A huge topic and one we’ll revisit in future newsletters. The enormous prevalence in females makes it a pain priority yet continues to be under-resourced and difficult to manage.
Chronic pelvic pain (CPP) in men is a significant yet often under-recognized health issue in Australia. Estimates suggest that up to 10% of Australian men experience CPP, encompassing conditions such as chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS). Discussion in the literature of classification shows a large phenotypic variability and likely causation.
The causes of male CPP are multifactorial and often elusive. Common contributors include pelvic floor muscle dysfunction, chronic prostatitis, urinary tract infections, and sexually transmitted infections.
Presentations of male chronic pelvic pain usually occur later in life in comparison to female pelvic pain. The site of pain is more commonly testicular, perineal rather than penile or rectal. Common symptoms include pressure, throbbing or burning pain in the above sites. In addition, patients report pain on sitting, walking, contact e.g. underwear and associated symptoms in bowel, bladder, urinary and sexual function.
Psychological factors such as stress and anxiety are also associated with the onset and persistence of symptoms. The condition's complexity necessitates a multidisciplinary approach to management, incorporating medical, physiotherapeutic, and psychological interventions, not least due to the effect of pain on self-esteem and socialisation including relationships. 1
Despite its prevalence, male CPP remains underdiagnosed and undertreated in Australia. Increased awareness and comprehensive management strategies are essential to address this multifaceted condition and improve the quality of life for affected individuals.
We would recommend pelvicpain.org.au as a useful resource for education and patient education of both male and female pelvic pain.
Non pelvic causes of pelvic pain
Quite correctly, pelvic pain needs proper assessment through history, exam and investigation. It’s worth considering in all cases that not all pelvic felt pain is originating in the pelvis and even if it is it may be from structures in the bony pelvis and not just the internal organs. The full extensive review of these is outside the remit of this but a couple of structures to commonly consider:
Facet referral patterns
Spinal bony referral
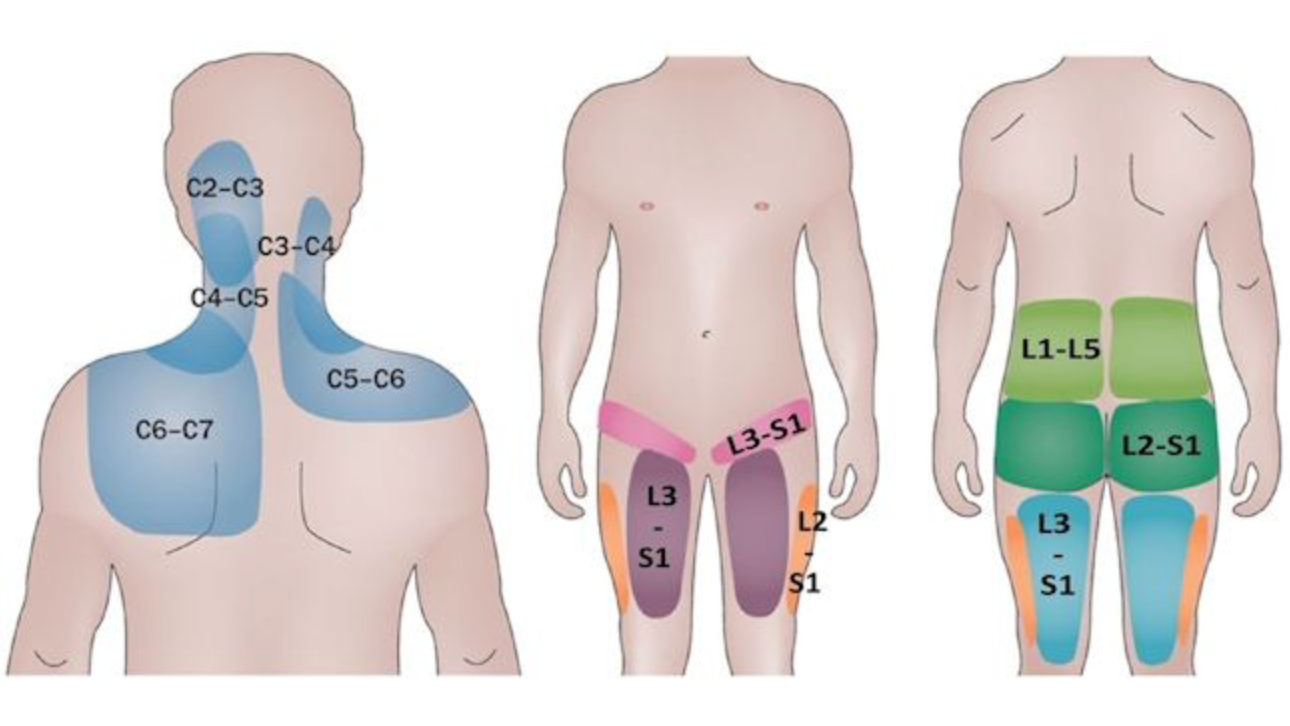
As per the attached image this simple representation just shows some of the projected referral patterns from facet arthropathy. Facet arthropathy according to some studies can account for lower back pain in up to 40% of cases of low back pain. 2 As we can see from these images though the facet joints refer pain pelvically. We recommend everyone with pelvic pain should have an assessment for a mechanical source of pain additionally. We wouldn’t recommend treating a scan result and particularly isolated single level unilateral facet injections – they are a poor indicator of pain causation and poor treatment option.
Other sources of pain include the sacroiliac joint, interspinous ligament and disc causation affecting the sacral nerve roots. From our experience the SIJ is a common cause of groin pain and therefore clearly hard to distinguish from pelvic causation.
Spinal radicular pain
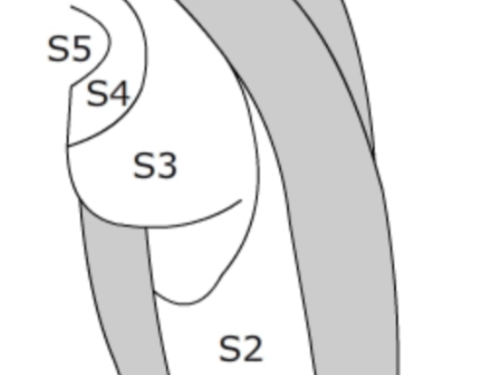
The second image shows the sacral dermatomes. Radicular pain is pain in the distribution of a nerve root so anything affecting the distal sacral nerve roots particularly will cause a pelvic pain by definition. In addition, a lot of rigidity is often applied when we think of dermatome mapping. It is our experience these are a guide only of where someone is likely to feel pain and not the crystal-clear demarcations we are taught at medical school.
Dermatomes of the upper leg and pelvis
Pudendal Nerve Block & Pulsed Radiofrequency
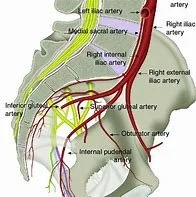
Important Anatomical Sites in the Punendal Nerve Pathway
What is it?
The pudendal nerve supplies sensation to the perineum, genitals, and anal region and plays a key role in pelvic floor motor function. Pudendal neuralgia can result in sharp, burning, or aching pain in these areas, often worsened by sitting. Pudendal nerve block is both a diagnostic and therapeutic tool, offering temporary pain relief and guiding further management. When symptoms persist despite conservative measures, pulsed radiofrequency (pRF) offers a minimally invasive, non-destructive option to modulate nerve activity and reduce pain.
When to refer?
Consider referral for pudendal nerve block and/or pRF when patients present with neuropathic perineal pain unresponsive to medications (e.g. amitriptyline, gabapentinoids) or pelvic physiotherapy. pRF is particularly useful in patients who have partial response to a diagnostic block, and in those unsuitable for more invasive surgical options. These procedures are image-guided (fluoroscopy or CT), outpatient-based, and generally well tolerated.
References:
Lai HH, Pontari MA, Argoff CE, et al. Male Chronic Pelvic Pain: AUA Guideline: Part I Evaluation and Management Approach. J Urol. 0(0). doi:10.1097
Du, R., Xu, G., Bai, X., & Li, Z. (2022). Facet Joint Syndrome: Pathophysiology, Diagnosis, and Treatment. Journal of Pain Research, 15, 3689–3710.